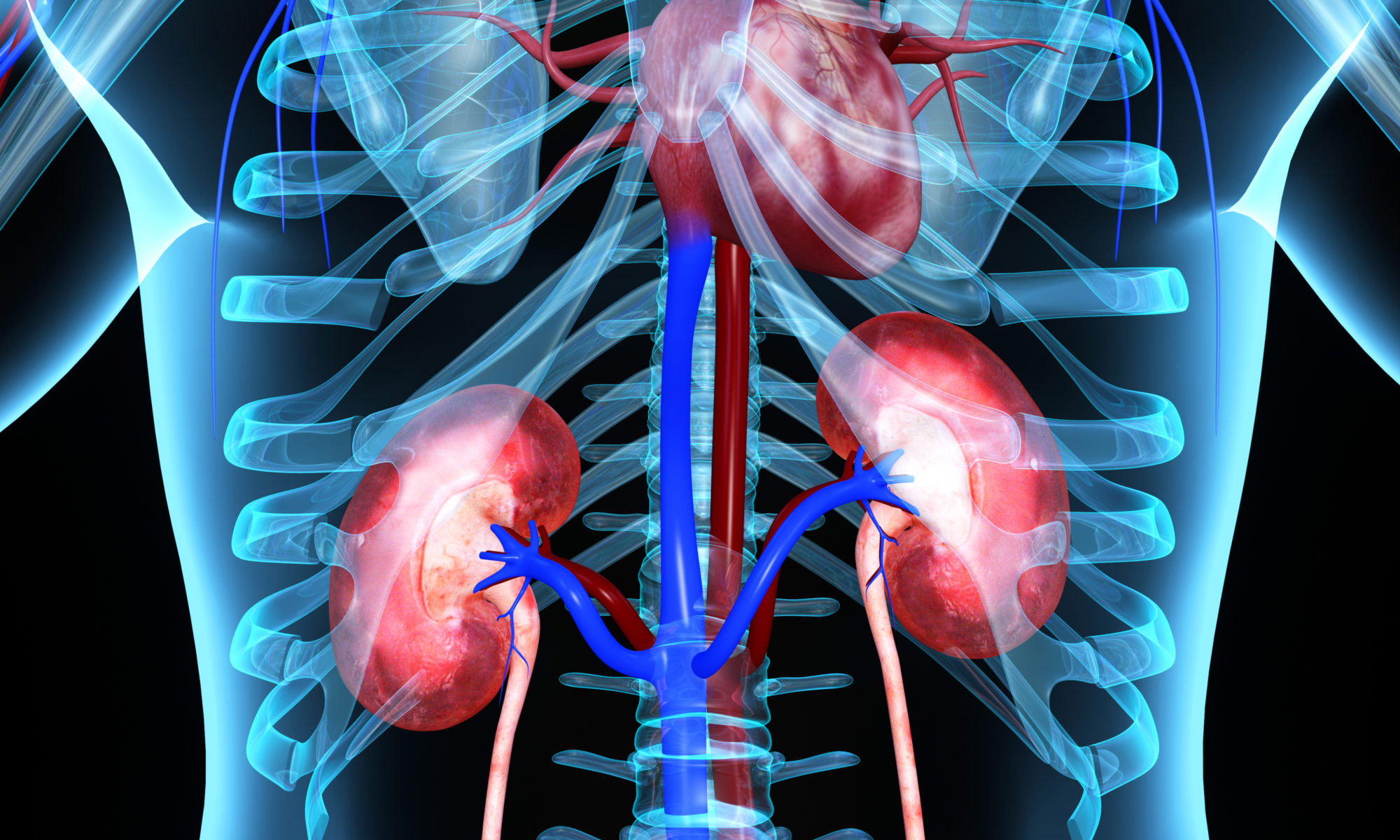
The new allocation system for donor hearts, implemented by the United Network of Organ Sharing (UNOS) and the Organ Procurement and Transplantation Network in 2018, improves access to donor hearts for critically ill candidates. This means patients are sicker at the time of transplant, which increases the likelihood of end-stage organ failure, especially the kidneys.
While multi-organ transplants are relatively rare, cardiac multi-organ transplants are increasing in frequency. To date, these procedures account for approximately 7 percent of all heart transplant procedures performed in the United States. Because multi-organ transplants are more difficult than individual transplants, they require the high level of medical expertise and surgical skills found at major transplant centers.
Call 214.820.6856 to refer a patient for heart transplantation or evaluation for a multi-organ transplant at Baylor Dallas
Shelley Hall, MD, FACC, FHFSA, FAST, Chief of Transplant Cardiology, Mechanical Circulatory Support and Advanced Heart Failure, Baylor University Medical Center at Dallas (Baylor Dallas), part of Baylor Scott & White Health and president of the Texas Chapter of the American College of Cardiology, and Timothy Gong, MD, FACC, Assistant Medical Director, Advanced Heart Failure Outreach, Baylor Dallas, recently authored updates to the American College of Cardiology’s Heart Failure Self-Assessment Program about when to proceed with multi-organ transplantation.
In addition, Dr. Hall serves as the cardiac representative on the UNOS multi-organ transplantation committee, which developed guidelines and criteria to standardize the transplant community’s approach to dual organ transplant. The guidelines were approved in June and will go into effect in 2023.
“As with so many issues in the transplant community, dual-organ transplantation stimulates a lot of debate and ethical discussions about what is fair in the allocation process,” Dr. Hall says. “Some may think kidney-only recipients are being disadvantaged as more organs are diverted to dual-organ recipients. But heart-kidney transplants, which are the most common dual-organ procedure involving the heart, have shown modestly improved outcomes with some increased survival benefit compared with heart transplant alone for patients with significant renal dysfunction.”
Multi-organ transplantation requires a strong level of coordination between the cardiac transplant team and the abdominal transplant team. As Baylor Dallas has become more sophisticated in expanding access to multiorgan transplantation, the teams have developed extensive protocols and well-defined processes by which the procedure occurs.
“Dual organ transplant involves very robust communication between both transplant teams, because sometimes not each individual surgery goes as smoothly as expected,” Dr. Gong says. “Both teams have to be prepared to make difficult decisions as to when it is safe to proceed. Some examples include when the transplanted heart is not functioning at the level expected or dangerously low blood pressure that could affect the new kidney. Communication among all the key players is so important because these patients are exceedingly complex.”
Future directions for multi-organ transplantation include further refinement of uniform criteria for all multiorgan candidacies, potential “safety-net” thresholds for transplanting the heart alone but allowing opportunity for high-urgency listing of the second organ should it fail, and moving toward equitable organ allocation for multiorgan transplant candidates.