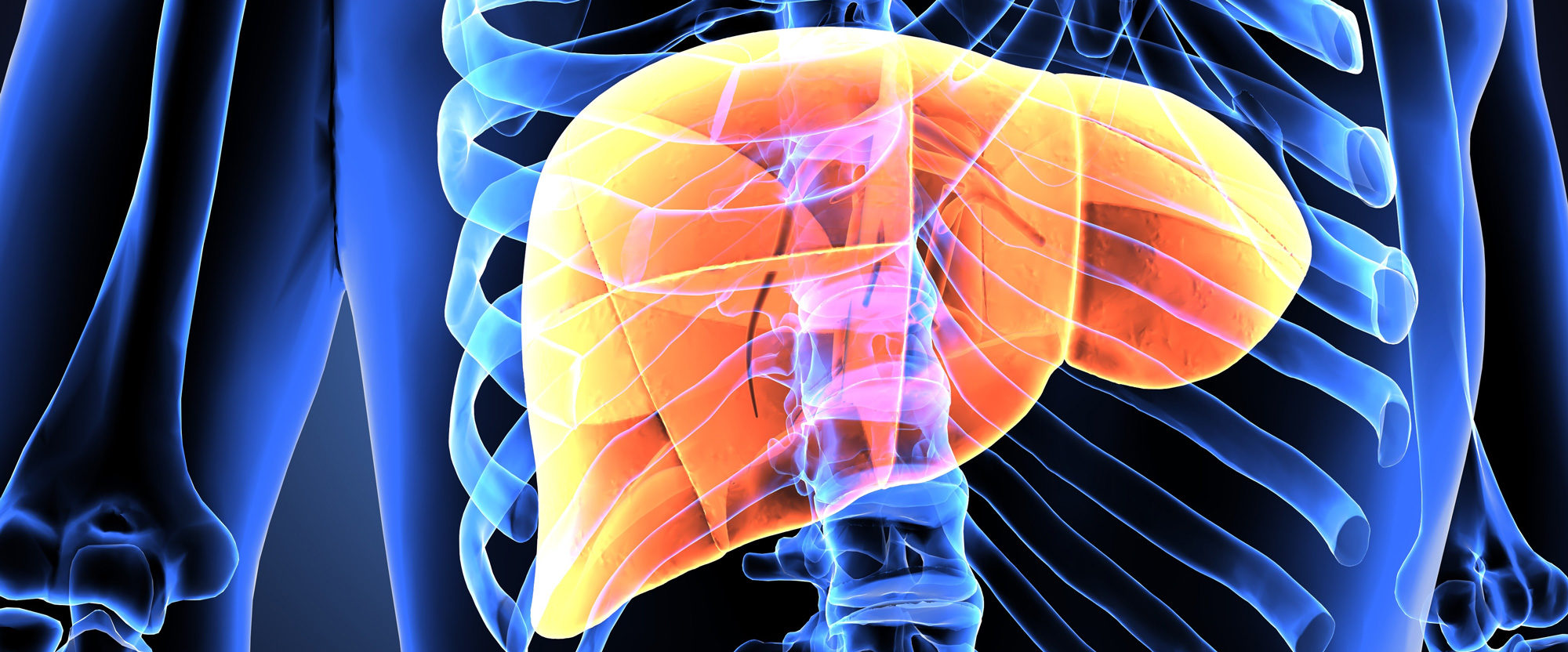
Liver disease is the eighth leading cause of death in the United States and the third or fourth leading cause of death among patients 45 to 64. To improve these outcomes, many hepatologists on the medical staffs of Baylor University Medical Center at Dallas and Baylor Scott & White All Saints Medical Center – Fort Worth are undertaking a number of notable patient-centered research projects. All research projects are administered by Baylor Scott & White Research Institute.
Using systemwide data from Baylor Scott & White Health, as well as data from other healthcare systems in Dallas/Fort Worth, Sumeet Asrani, MD, MSc, Director of the Center for Advanced Liver Disease at Baylor Dallas, showed that the burden of liver disease is increasing at a faster rate than heart failure and is disproportionately affecting the elderly.
“The rise in fatty liver disease and the incidence of hepatitis C among baby boomers accounts for much of this increase,” Dr. Asrani says. “This has implications for how we manage our Medicare population as the number of liver patients above the age of 65 is going to increase.”
Based on these results and the system’s emphasis on pursuing this type of research, Baylor Dallas is already pursuing involvement in additional studies that look at quality of care and metrics for effective management of patients with cirrhosis.
Studies of kidney function and liver disease
For patients who have undergone liver transplant, chronic kidney disease is a major challenge. Many immunosuppressive medications are nephrotoxic. And patients undergoing transplant are often older and sicker, putting them at greater risk of complications. Using the resources of the robust Baylor Scott & White Health liver transplant database, the researchers devised a new equation to estimate kidney function in patients with liver disease. To further study renal function, in a collaborative study with Northwestern University, and using the transplant biorepository, they were able to identify and validate novel biomarkers to predict renal failure after liver transplantation.
“We are really good at getting patients through transplant,” Dr. Asrani says. “We have one of the highest success rates in the country. As we improve mortality, we want to also improve morbidity so patients can lead longer, healthier lives.”
Researchers at Baylor Scott & White Health are also participating in several pivotal trials of fatty liver disease, including one that was published in The Lancet, to treat nonalcoholic steatohepatitis or NASH.
“Sixty million people in the U.S. have fatty liver disease, and of these, 500,000 will end up with cirrhosis. Yet many have never had a drink in their life,” says James Trotter, MD, chair, transplant hepatology, Baylor Scott & White Health. “While much of cirrhosis is related to alcohol and hepatitis, we are now seeing an increasing number of patients with liver disease due to lifestyle factors, like obesity and liver disease.”
Additional studies include participation in a prospective multicenter study looking at the causes of recurrence of fatty liver disease after liver transplantation. Such studies are possible as a result of the close working relationship between hepatologists and liver transplant surgeons on the medical staffs that allows patients to be closely followed after transplant in an effort to keep them healthy.
Hepatologists are collaborating with transplant nephrologists in a study to look at the role of cystatin C, a novel biomarker as an alternative to serum creatinine to measure kidney function in patients with cirrhosis and liver failure. Baylor Scott & White also is playing a predominant national role in a multicenter trial studying treatment of hepatorenal syndrome.
Baylor Dallas was the top enrolling site out of 125 international sites registered to study a new drug targeting ammonia to improve hepatic encephalopathy, a complication of end-stage liver disease. The current phase 2 and future phase 3 studies into hepatic encephalopathy will be conducted at Baylor Dallas.
“Patient-centered research is vital to our mission of helping to advance the field and improve the quality of care we provide to our patients,” Dr. Asrani says. “Access to a robust transplant biorepository and prospective database that has been meticulously built over the last 30 years, fruitful collaborations with our colleagues in transplant surgery and health services research, and access to stellar colleagues across specialties allows us to engage in collaborative research.”