Each year in the United States, approximately 600,000 people have a pulmonary embolism, with an estimated 50,000 to 200,000 dying from the condition. Because of the high mortality rate associated with massive and sub-massive pulmonary embolism, identification and early intervention are critical. Yet, this common condition remains underdiagnosed and undertreated.
The dedicated Pulmonary Embolism Response Team (PERT) at The Heart Hospital Baylor Plano is focusing on these often-preventable deaths and working to improve long-term outcomes for patients experiencing massive and sub-massive pulmonary embolism. Currently, the hospital is the only location in North Texas with a formalized team ready to accept transfers of complicated patients with this life-threatening condition.
Bringing Together Multiple Disciplines
Since the PERT was created two years ago, the hospital has taken a streamlined approach to pulmonary embolism care through its multidisciplinary team. Together, physicians on the medical staff from multiple specialties make critical decisions to determine the appropriate treatment for each patient, such as medical management, inferior vena cava filter, catheter-directed intervention, clot removal, systemic thrombolytics or surgery.
“Over the last five to seven years, the science of cardiovascular disease has been shifting toward a team approach in every aspect,” said Sameh Sayfo, MD, an interventional cardiologist on the medical staff at Baylor Scott & White The Heart Hospital – Plano. “For pulmonary embolism, you need multiple specialists to be involved.”
To help expedite care, physicians on the medical staff specializing in emergency medicine, pulmonary/critical care, interventional cardiology, vascular surgery and cardiovascular surgery, as well as nurses, cath lab staff and perfusionists, are ready to mobilize. To support the team and the increased level of care provided, the hospital has also invested in upgraded equipment and advanced skills for ancillary staff.
“The best way to get pulmonary embolism patients treated using best practices is to get all of the players on the same team, which is what the PERT does,” said William Shutze, MD, a vascular surgeon on the medical staff at Baylor Scott & White Heart – Plano. “We can quickly stratify people into whether they have a low-risk PE, sub-massive PE or massive PE and follow the protocols to treat them efficiently.”
Sub-Massive Pulmonary Embolism
For those with sub-massive pulmonary embolism, the team brings together expertise to guide decisions on traditional management with anticoagulants or treatment using percutaneous intervention. For appropriate patients, percutaneous intervention can address oxygenation problems, reduce the strain on the heart and provide a significant difference in long-term quality of life.
Many patients treated with anticoagulants alone will return with complications later, such as a right ventricular failure or pulmonary hypertension. At that point, these patients require chronic oxygen and have limited treatment options.
“A lot of patients don’t get the treatment they deserve because the facility where the patient goes isn’t aware of it, or they are under old mentality of just putting the patient on Heparin,” Dr. Sayfo said. “Initially, the patient may do well, but if you follow that patient long-term, he or she doesn’t always do as well.”
In a recent PERT case, a patient with chronic lung disease, who was on daily oxygen, began experiencing increasing shortness of breath. The patient arrived at the emergency room with a bilateral pulmonary embolism. Through the multidisciplinary team, an interventional cardiologist along with a pulmonary specialist assessed the patient, who met the criteria for a catheter-directed TPA device. Following the procedure, the patient was able to walk 400 feet with no oxygen at all.
“When we do these procedures, in addition to preventing patients from having long-term complications, the patients usually go home sooner,” Dr. Sayfo said. “Many patients go home the next day, with an average hospital stay around three days. When a sub-massive pulmonary embolism is treated the traditional way, patients may stay in the hospital five to seven days.”
Massive PE
Typically, those with a massive pulmonary embolism are not candidates for treatment using percutaneous intervention. The dedicated PERT at Baylor Scott & White Heart – Plano allows these patients to receive rapid, quality care from cardiovascular surgeons who perform surgery to remove the clot.
“Our goal for patients who have a massive pulmonary embolism is to reduce mortality,” Dr. Shutze said. “Right now, mortality for these patients is 30-50 percent. We’re trying to get that as low as possible.”
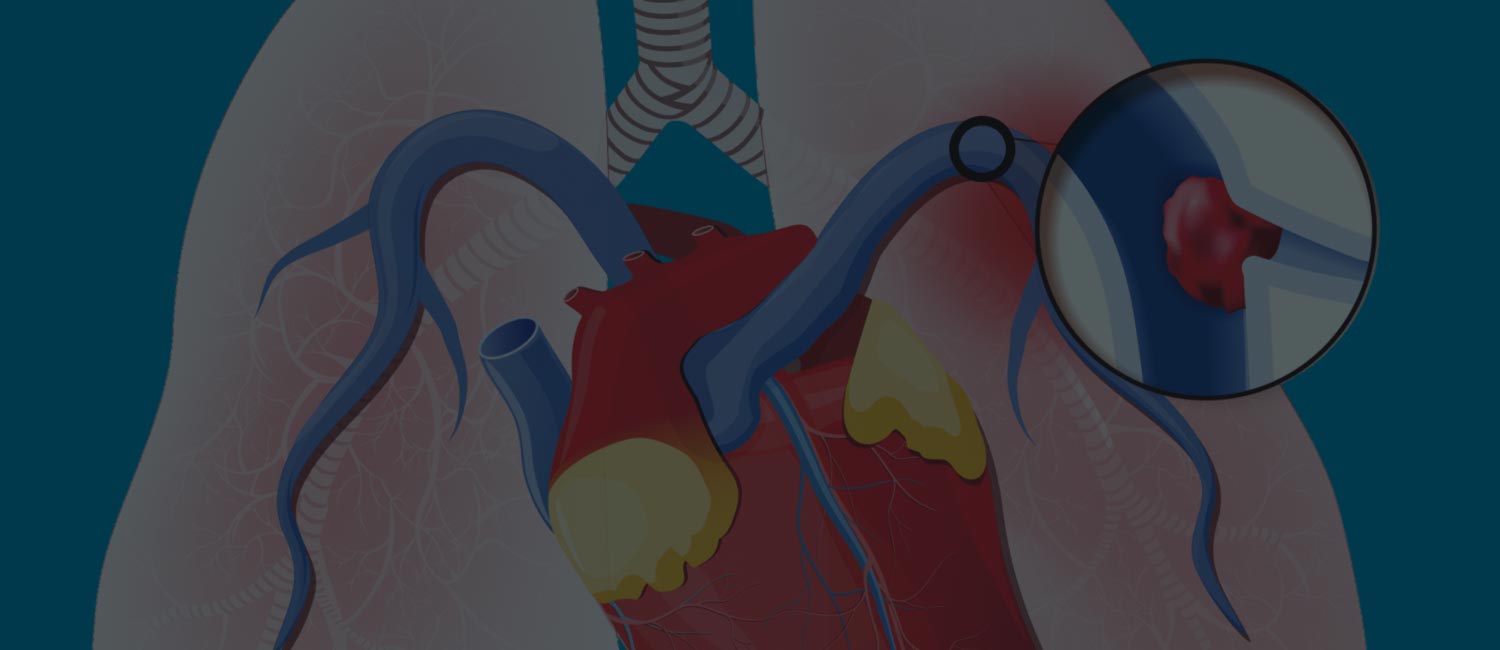
In a recent PERT case, a patient presented with acute shortness of breath and low oxygen, and a CT scan revealed a massive pulmonary embolism. An echocardiogram showed a very large thrombosis in the right atrium of the heart, which is a contraindication for percutaneous intervention. Through the team, a cardiothoracic surgeon was able to operate, removing a 13-centimeter clot from the heart and a 9-centimeter clot from the lungs. After surgery, the patient was able to go home in just a few days.
Advancing PERT
As the team provides a multidisciplinary approach to pulmonary embolism care, the hospital will continue to evaluate patient outcomes and define processes for these patients. To track outcomes, the team recently started research data collection.
“Every PERT team has a little bit different protocol,” Dr. Shutze said. “Each team has a responsibility to do a continuous quality improvement process, look at the results and fine-tune the process. We’ve already been doing that.”
Physicians are also using the protocols established for pulmonary embolism and applying them to efficiently treat other conditions. For example, the team follows similar processes for evaluation and treatment of deep vein thrombosis (DVT).
24/7 Pulmonary Embolism Care
The PERT is available 24/7 for emergent transfers of patients needing rapid evaluation and treatment. However, it is not just for acute cases. It is also available for any pulmonary embolism patient who may benefit from evaluation by a multidisciplinary team, including in the outpatient setting.
“We can transfer patients who require a higher level of treatment or, for those needing outpatient evaluation, see them as an outpatient,” Dr. Sayfo said. “Together, we can help get patients the better quality of life they deserve and lower the chance of later complications that aren’t reversible.”