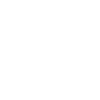
Prevalence of the bone infection osteomyelitis (OM) has increased along with the increased prevalence of diabetes. It is estimated that OM is a complication for at least 10% of diabetic foot ulcers and approximately 50% of severe cases. Delays in the diagnosis and treatment of OM can lead to poor patient outcomes and high healthcare costs. However, an accurate and timely diagnosis of OM is hindered by a lack of clear guidelines for histopathological assessment. Therefore, researchers from Baylor Scott & White Research Institute, along with their collaborators, have created a new diagnostic framework for OM.
Their report, published in the March-April 2020 issue of the Journal of Foot and Ankle Surgery, describes the creation and testing of an algorithm for differential diagnosis of OM categories.
Using the literature as a guide, the team created an algorithm for OM classification. They first established 15 histological features of OM, including detailed descriptions and guidance for differential diagnosis. They then weighted the criteria as major, intermediate, and minor for either acute or chronic disease. Next, they established five diagnostic categories of OM, which could be derived from the profile of histological features from each specimen. These included the previously recognized categories of acute OM (AOM), chronic OM (COM), and acute and chronic OM (ACOM). They also found evidence to support the existence of two new categories: chronic active OM (CAOM), and chronic inactive OM (CIOM).
They tested their algorithm using samples from 263 patients with suspected OM in the distal lower extremity for whom sufficient clinical information and tissue samples were available. They recorded the presence or absence of each diagnostic criterion, determined a diagnosis, and calculated a histopathological load score, known as a Jupiter Score, which was the sum of scores from all criteria.
They found that for 44.6% of the patients, the original diagnosis was negative, and the criteria-based diagnosis was positive, indicating that these patients may have been underdiagnosed. In support of this, they found that more patients experienced nonhealing wounds and further complications in the group with non-concordant diagnoses than in the group with concordant diagnoses.
Overall, their research supports the consensus that OM is a dynamic, progressive process, which involves a set of defined histopathological changes. For instance, AOM is characterized by the destruction of bone, whereas COM is characterized by remodeling of bone. Furthermore, AOM is thought to progress to COM. The use of an algorithm-based diagnostic tool can potentially improve the accuracy and consistency of clinical diagnosis.
The researchers hope that this diagnostic tool will improve diagnostic agreement among pathologists, which is currently at 30%. Furthermore, these changes may help clinicians to direct treatment more accurately, thus avoiding lower limb amputation.
BSWRI researchers associated with this work include Arundhati Rao, MD, chair of Pathology at Baylor Scott & White Health at Temple, TX, V.O. Speights, DO, pathologist at Baylor Scott & White Health at Temple, TX, and the lead author, Amelia Sybenga. Dr. Sybenga was a pathology resident and fellow with Baylor Scott & White during this study and is now a faculty member at the University of Vermont. Dr. Speights passed away during this study. He is remembered for his compassion and dedication to advancing the pathology profession both locally and nationally.